Developing a participatory approach to the systems improvement of traumatic brain injury care in Yangon, Myanmar
Trauma accounts for nearly 10% of global deaths, of which 90% occur in low and middle income countries (LMICs). Traumatic brain injury (TBI) is one of the most devastating, both in terms of mortality, but also in terms of the long-term implications to both the patient and their family.1,2
Caring for the TBI patient is a complex task, involving a number of different heath system elements: pre-hospital care, emergency medicine, anaesthesia, surgery, intensive care, physiotherapy, and rehabilitation. These elements are inter-dependent, and improving one area may not show a measurable benefit without concomitant improvement in the others. Furthermore, TBI care is context-specific with lessons from one setting not easily translating to a new environment. This variation does not simply apply to the technical expertise required but to the fundamental questions if what constitutes an acceptable final outcome.3
Healthcare is the emergent property of a sociotechnical system consisting of people, processes, information, equipment, consumables, infrastructure, culture, finance, and governance. To improve the overall care of TBI patients, we need to understand how these come together how these deliver the existing system of care, and how specific interventions might work to reengineer them to provide the desired system of care. This requires a health systems approach.
Systems thinking is championed in healthcare by the World Health Organisation (WHO), the Institute for Healthcare Improvement (IHI), and many others. The WHO specifically recommend its place in LMIC healthcare improvement given the complexity of this undertaking.4–6 In considering TBI, the need for a systems approach is also advocated by both the Lancet Commission for Global Surgery and the Lancet Neurology Commission on TBI.7,8 However, there are few examples of a systems approach being applied to TBI care in LMICs.
A new position document published by the UK Royal Academy of Engineering in partnership with the Royal College of Physicians and the Academy of Medical Sciences has demonstrated the value that the Engineering community can add to the understanding and improvement of complex healthcare systems.9 (Fig 1). We have established a partnership between clinical academics in the UK and Myanmar with an interest in Neurotrauma, alongside the Healthcare Design Group, based in the Engineering Design Centre, Cambridge. This partnership is seeking to use tools from the engineering community to understand the current service around TBI care in Myanmar, and to understand how interventions may be designed to improve this service.
The project is beginning with a qualitative exploration of the current experiences of TBI in Myanmar through a variety of stakeholders. This will be performed through facilitated interviews conducted by our partner researchers in Myanmar, and seek to explore some core questions relating to the provision of TBI care (Fig 2):
- Who are the stakeholders?
- Where is the system of TBI care situated?
- What are its elements?
- How does the system perform?
Using this data we will then seek to develop consensus models which can help describe the current system of TBI care in Myanmar and inform the design of a series of interventions to improve TBI care which are context-dependent, and consistent both with each other and with the wider heath system.
Fundamental to this approach is that it is context-specific: carried out by Myanmar researchers and seeking to explore the perspectives of not only clinicians but also clinical managers, patients and the public.
References
- Lozano, R. et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2095–2128 (2012).
- Murray, C. J. L. et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2197–2223 (2012).
- Rubiano, A. M., Carney, N., Chesnut, R. & Puyana, J. C. Global neurotrauma research challenges and opportunities. Nature 527, S193–S197 (2015).
- Adam, T. & De Savigny, D. Systems thinking for strengthening health systems in LMICs: Need for a paradigm shift. Health Policy Plan. 27, 2006–2008 (2012).
- Rwashana, A. S., Nakubulwa, S., Nakakeeto-Kijjambu, M. & Adam, T. Advancing the application of systems thinking in health: understanding the dynamics of neonatal mortality in Uganda. Heal. Res. Policy Syst. 12, 36 (2014).
- Adam, T. et al. Evaluating health systems strengthening interventions in low-income and middle-income countries: Are we asking the right questions? Health Policy Plan. 27, (2012).
- Meara, J. G. et al. Global Surgery 2030: Evidence and solutions for achieving health, welfare, and economic development. The Lancet 386, (2015).
- Maas, A. I. R. et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 4422, (2017).
- Engineering better care: a systems approach to health and care design and continuous improvement. Royal Academy of Engineering, Academy of Medical Sciences, and Royal College of Physicians. (2017).
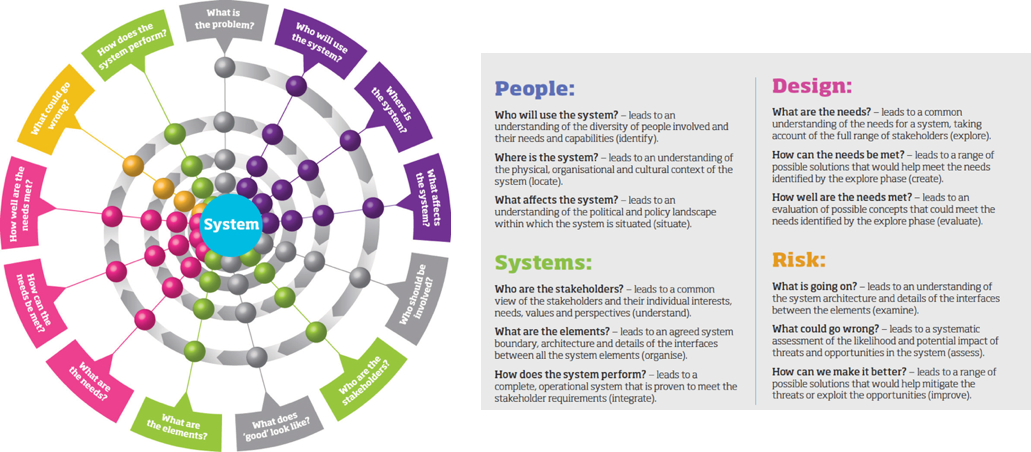
Reproduced with permission from Engineering better care. Royal Academy of Engineering, Academy of Medical Sciences and Royal College of Physicians. 2017